Expert CornerArticle from the SICOT Knee Arthroplasty Subspecialty Committee: | ||
Francesco Benazzo |
L. Perticarini | |
SMP Rossi | ||
Constraint can be defined as “the state of being checked, restricted, or compelled to avoid or perform some action” (Merriam Webster Dictionary). In the knee prosthetic world, this means that the two components, femur and tibia, are linked together in different degrees according to the need of the knee itself, to provide the sufficient stability not given by ligaments, capsule, and extensor mechanism. The term constraint is improperly extended to unconstrained design, such as CR and PS, which dictates the way the new joint moves (kinematic), but they do not provide any additional stability, which is given by the capsule and by the level of conformity between femoral component and liner.
The choice of the level of constraint in primary knee arthroplasty should be based on different variables, namely age, gender, BMI and level of activity of the patient, degree and location of the deformity (intra/extra-articular), the ligaments and capsule competence, and finally the confidence of the surgeon with different implants and a suitable technique.
The lowest level of constraint, or natural constraint given by the presence of the central pivot and capsule, is represented by unicompartmental implant, or the combination of 2 of these implants (bicompartmental). In this case the natural stabilizers are all preserved and so the proprioception of the patients. This solution leads to very interesting results and patients’ satisfaction as demonstrated by many papers. The combination of two small implants to address more than one compartment can be technically demanding and should be performed by experienced surgeons.
One or both of the natural major constrainers (ACL and PCL), are absent in CR (ACL) and PS (both). Stability is provided by the capsule, the extensor mechanism, and by the reciprocal conformity of the components. The choice of preserving or sacrificing the PCL, with a Cruciate Retaining (CR) or a Posterior Stabilized (PS) implant, is still controversial, and in the literature, there is no consensus on which implant is superior to the other. The choice can be therefore related to different variables such as surgeon preference, surgical technique and patients’ characteristics.
CR implants have the advantage of saving bone, as no box for the Cam-Post mechanism is needed. This could be advantageous in young patients and active patients or in patients, especially women, with small femora, where a box would be relatively big if related to the dimension of the femur. Most of the manufacturers are also now improving their implants giving the possibility to choose alternative bearings such as ultra-congruent or medial-pivoting liners that are also compatible with a release of the PCL, sometimes needed to better balance the knee or to avoid a flexion contracture, and where constraint is given by the high level of conformity (dished liners). On the other side, in modern PS implants the box is becoming relatively smaller, with a reduced sacrifice of bone and the surgical technique can be easier in terms of ligament balancing and treatment of a flexion contracture with also a reduced long term risk of instability due to PCL failure.
Both CR and PS implants should be used in knees with correctable deformities and good ligament status, with no need of extensive releases that may reduce the final stability of the implant.
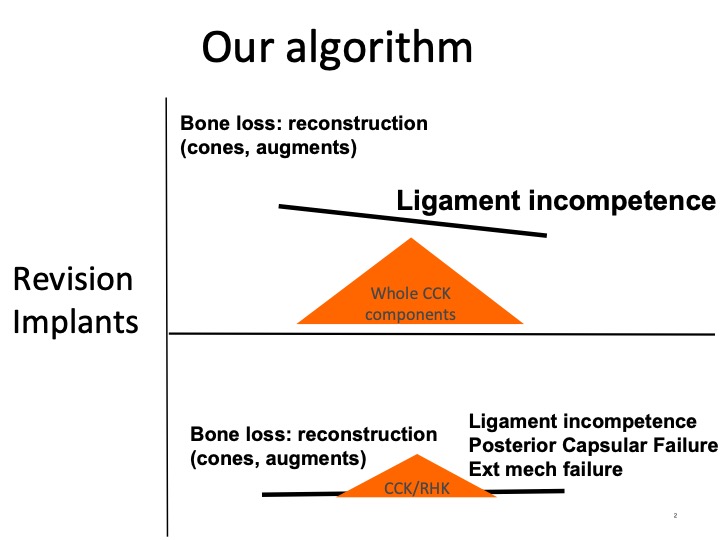
Ligament incompetence or extensive releases are the main reasons to upgrade the constraint. In the past, this required in the majority of cases the Varus-Valgus constrained (VVC) implant, which implies the use of stems and the sacrifice of a bigger amount of bone to accommodate the box for the cam-post mechanism using a wider polyethylene post that closely conforms to a large femoral component box. Increased stability is achieved by limiting varus-valgus and torsional movement, the extent of which varies across different designs. Before the need of choosing VVC implant such as a Condylar Constrained Knee (CCK), an intermediate option is now available for some implants. These mid-level constrained implants, are basically PS implants with a higher level of constraint due to a wider post than a standard posterior stabilized (PS) insert, but a narrower and shorter post than a CCK insert, thus conforming to standard PS femoral boxes but reducing the level of freedom.
The possibility of using a middle range constraint mechanism, could be a solution in most primary cases, where a CCK liner has been used so far. Particularly in those cases where, despite the adoption of a properly performed surgical technique, we can expect a residual varus-valgus laxity, addressable with primary implants and a middle range constraint system. The clear advantage is the reduced removal of bone from the femur compared to CCK, and the use of primary components.
Some patients could also like the feeling of stability given by a guided motion.
Finally, more constrained implants such as VVC implants should be used in case of major deformities with complete ligament incompetence or failure, and/or bone losses requiring the use of augments sleeves or cones incompatible with a lower constrained implant (unless the use of a PS liner with a CCK implant will result in a well-balanced knee).
Rotating Hinged (RH) Implants have little role in primary knee arthroplasty. They can find place in older patients, in post-traumatic cases or in severe deformities where the ligament competence, once the deformity is addressed, is doubtful.
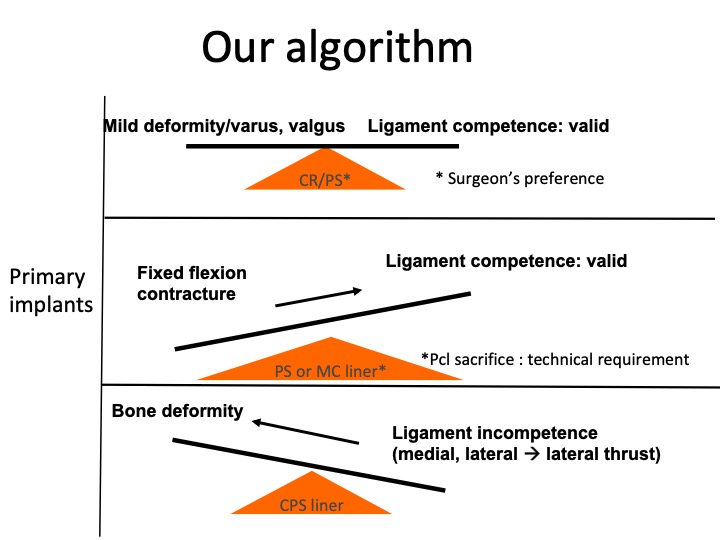
MC liner = Medial Congruent
- Kennedy JA, Burn E, Mohammad HR, Mellon SJ, Judge A, Murray DW.
- Lifetime revision risk for medialknee replacement is lower than expected. Knee Surg Sports Traumatol Arthrosc. 2020 Feb 12. doi: 10.1007/s00167-020-05863-3. [Epub ahead of print]
- Migliorini F, Eschweiler J, Tingart M, Rath B.
- Posterior-stabilized versus cruciate-retained implants for total knee arthroplasty: a meta-analysis of clinical trials. Eur J Orthop Surg Traumatol. 2019 May;29(4):937-946. doi: 10.1007/s00590-019-02370-1. Epub 2019 Jan 16.
- Indelli PF, Morello F, Ghirardelli S, Fidanza A, Iannotti F, Ferrini A. No clinical differences at the 2-year follow-up between single radius and J-curve medial pivot total knee arthroplasty in the treatment of neutral or varus knees. Knee Surg Sports Traumatol Arthrosc. 2020 Feb 13. doi: 10.1007/s00167-020-05854-4. [Epub ahead of print]
- Badawy M, Fenstad AM, Furnes O. Primary constrained and hinged total knee arthroplasty: 2- and 5-year revision risk compared with unconstrained total knee arthroplasty: a report on 401 cases from the Norwegian Arthroplasty Register 1994-2017.
- Acta Orthop. 2019 Oct;90(5):467-472. doi: 10.1080/17453674.2019.1627638. Epub 2019 Jun 18.