
Expert Corner
AB-cemented Interlocking in Patients with Infected Non-Union of Lower Extremity
 Pavel Volotovski Pavel VolotovskiSICOT Associate Member - Minsk, Belarus |
Introduction
Infected non-union means not only bacterial inflammation and impossibility of weight-bearing, but also restricted range of motion and compromised soft-tissues as a result of trauma and previous surgeries. However, treatment of such cases presents two main problems for the surgeon – infection and fracture. In the presence of infection, the removal of the implant is mandatory to reduce the biofilm load and thus increase the probability of a permanent cure. However, to promote bone healing and achieve union we must stabilise the fracture. There are several options to choose from. Plating and nailing provide good stability, but require staged procedures and lead to a high risk of repeated infection. External fixation, on the other hand, can be associated with pin site infections and soft tissue scarring by pins and wires causing muscle contractures and joint stiffness. Also, this method is not possible in non-compliant patients. In ideal circumstances, the treatment should include a one-stage procedure providing good bone stability and a high local concentration of the appropriate antibiotic. In our institution, we use custom made locked intramedullary nails coated with PMMA-cement mixed with an antibiotic.
Surgical Procedure
As in the other cases, thorough preoperative planning is extremely important. Before the operation, we must predict the extent of debridement and possible correction of existing deformities, determine nail length and thickness, access locking possibilities and identify other risks to be encountered. It is crucial to obtain pre-op culture and sensitivity profile, because we need to choose both local and systemic antibiotics.
The patient is positioned and draped for tibial or femoral nailing depending on the segment of interest (e.g. Fig. 1).

Figure 1: Patient positioning for nailing of the tibia
The non-union area is opened and we need to perform thorough debridement of the infected bone and soft tissues followed by lavage with plenty of fluids. All the non-viable and infected tissues undergo debridement until bleeding viable tissue is present at the resection margins (“paprika sign”). Debridement is essential to prevent the recurrence of infection and biofilm formation, which protects the pathogens from antibiotics and host defense mechanisms. At this stage, we need to take specimens of the bone, soft tissues and any purulent material and send them for aerobic and anaerobic cultures.
The coating of the nail is prepared under sterile conditions at the back table. The materials required to prepare the cement nail include one package of gentamycin-impregnated bone cement; PVC tube of the appropriate diameter (2-3 mm more than the diameter of the nail); solid interlocking nail; 2 g of vancomycin (or other thermostable antibiotic according to the predetermined sensitivity) powder per 40 g pack of polymethylmethacrylate.
 a |  b |
 c |  d |
 e |  f |
Cut the PVC tube to appropriate length (Fig. 2-a). Tube cuttings can be used to fill the locking holes of the nail – it will facilitate drilling after cementing (Fig. 2-b). Mix one pack of 40 g bone cement with the antibiotic to obtain a homogenous powder. Add liquid monomer and mix. The cement is injected into the PVC tube in a highly viscous stage using a cement syringe or cement gun (Fig. 2-c). The nail attached to the guide is gently inserted into the tube. The tip of the nail should be free of cement, because it simplifies nail insertion to the intramedullary canal and prevents mantle disruption. Once the antibiotic nail has hardened and cooled, the tube is cut longitudinally with a scalpel and gently stripped off in a manner similar to peeling a banana (Fig. 2-d). The holes for locking screws are drilled (Fig. 2-e). When the nail is ready (Fig. 2-f), it can be inserted into the prepared intramedullary canal.
Usually it takes about 30 minutes to prepare the antibiotic cement-coated nail from setting up the back table to insertion. One surgeon prepares the antibiotic-coated IM nail while anaesthesia is being induced and the assistant surgeons are preparing the patient. The surgeon and assistant, who take part in the debridement procedure, change gowns and gloves before the “clean” part of the surgery.
The IM canal is reamed 2 mm more than the diameter of the antibiotic cement-coated nail. The nail is not cannulated, so we do not use guide wire. Since the non-union site is exposed during the debridement process, the IM nail can be inserted across the site of non-union using direct visual inspection, palpation, and fluoroscopy. The nail is inserted in the standard fashion similar to any interlocking nail and locked proximally and distally to improve bone stability, both axial and rotational. Intraoperative fluoroscopy is used for confirmation of a satisfactory nail position.


Figure 3: Fragments of broken cement mantle and “debonded” nail
It is better to insert the nail by hand and not to use a hammer, because cement mantle can break off and remain in the canal (Fig. 3). “Cement-nail debonding” can also be prevented by adequate over-reaming of the canal. However, if this does occur, the debonded cement should be removed and new antibiotic cement-coated nail should be prepared and used.
After the surgery, the patient receives intravenous antibiotics based on cultures; typically parenteral antibiotics are given for 2 weeks followed by 4-6 weeks of oral antibiotics. The external immobilisation is not used, so early mobility of adjacent joints is possible immediately after procedure. Toe touch or partial weight bearing is allowed depending on fracture pattern. Follow-up includes CBC, ESR, and C-reactive protein for activity of infection.
If removal of an antibiotic cement-coated IM nail is indicated due to recurrent infection or other reasons, it can be performed in a standard fashion. If debonding does occur, the cement mantle can be removed from the canal using instruments, which usually are used for cement removal in revision after cemented total joint replacements.
Results
In the series of 41 patients (23 femur and 18 tibia) treated in our institution from 2009 to 2014 we achieved bone union in 87.8% patients and all 41 patients were full weight-bearing. Of course, every method has complications, and in 5 cases X-ray has not revealed evident consolidation, but 3 of them achieved bone union after repeated surgery with autologous bone grafting. Open fistulas were found in 6 (14.6%) patients and required hardware removal and debridement. Mantle fragmentation was revealed in 4 (9.7%) cases.
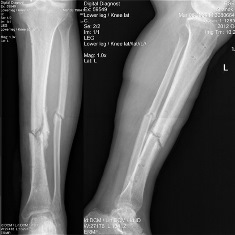

Figure 4: X-ray of patient Z with infected tibial non-union. Pre-op (8 months after initial nailing of open fracture) and 6 months after AB-cement nailing
Conclusions
There were several studies describing combination of an IM nail with gentamicin beads or antibiotic-impregnated cement inserted into the site of infection for treatment of infected non-unions [4]. The use of rods coated with antibiotic-impregnated cement prepared by using chest tubes was reported as the first-stage treatment [5,6]. However, these techniques require additional procedures for removal of the cement beads or removal of the cement-coated rods after 6 weeks and insertion of IM nails for providing non-union stability. Our technique combines 2 procedures into one surgery. A very similar treatment procedure has previously been reported to have a high rate of success [7]. This method can be effectively used for maintaining patients’ activity and mobility. It is quite simple and provides the possibility of early functional treatment.
- Trampuz A, Zimmerli W. New strategies for the treatment of infections associated withprostheticjoints.CurrOpinInvestDrugs2005;6:185–90.
- Patzakis M, Zalavras C. Chronic posttraumatic osteomyelitis and infected nonunion of the tibia: current management concepts. J Am Acad Orthop Surg 2005;13:417–27.
- Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104
- Sundgren K. Cemented modular intramedullary nail in failed knee arthroplasty: a report of 2 cases. Acta Orthop Scand. 1999;70:305–307
- Qiang Z, Jun PZ, Jie XJ, et al. Use of antibiotic cement rod to treat intramedullary infection after nailing: preliminary study in 19 patients. Arch Orthop Trauma Surg. 2007;127:945–951.
- Paley D, Herzenberg JE. Intramedullary infections treated with antibiotic cement rods: preliminary results in nine cases. J Orthop Trauma. 2002;16: 723–729
- Thonse R, Conway J. Antibiotic cement-coated interlocking nail for the treatment of infected nonunions and segmental bone defects. J Orthop Trauma. 2007; 21:258–68.

















