How I do a Primary Total Knee Arthroplasty
Amar S. Ranawat Hospital for Special Surgery, New York, United States Co-author: Peter B. White |
Introduction
Total knee arthroplasty (TKA) is well known as one of the most successful and widely performed operations for relieving pain and improving function. The success of this operation is highly dependent on the appropriate soft-tissue balancing, accurate component positioning and adequate pain control.
Over the past few decades, there have been several advances in soft-tissue balancing and pain management. With respect to gap-balancing, our institution has made several modifications to the originally described flexion-first method. We typically balance TKAs in extension first, making use of the 'inside-out' technique for cases of severe deformities [1, 2]. For the flexion-gap, we perform the so-called 'parallel to the tibial cut' technique [3].
Adequate pain control is achieved by using a multimodal pain protocol highlighted by preemptive analgesia, a series of periarticular injections and a postoperative analgesic regimen, which targets different nocioreceptors [4, 5, 6].
With these soft-tissue balancing and pain management techniques, we have had excellent clinical results. This article will outline our clinical experience and techniques in achieving a successful TKA.
The Operation
After thorough preoperative planning, a combined spinal and epidural regional anesthesia is administered to the patient usually in conjunction with a saphenous nerve block. A medial parapatellar approach is performed in flexion without the tourniquet using electrocautery to achieve hemostasis. Once the articular surfaces have been adequately exposed, the tibia is subluxed and hyperflexed in front of the femur using the 'Ran-Sall' technique.
Then using an extramedullary alignment guide, the tibia is cut perpendicular to its long axis, removing approximately 8-10 mm of bone from the unaffected side. In cases of severe deformities, we may cut slightly less bone (6 to 8 mm), always at 90° to its long axis. The tibial component is then sized and lateralized. Osteophytes are removed and occasionally a reduction osteotomy is performed to remove excess bone.
When preparing the femur, we prefer to use an intramedullary guide for alignment. In cases of lesser deformities, we aim to resect the distal femur in 5° of valgus, however, in cases of severe deformities (i.e. Type II or III valgus), this angle can be adjusted to 3° with a resection of slightly less than the usual 10-mm.
At this point it is necessary to correctly balance the knee starting with the extension-gap. In cases of severe deformities we use the 'inside-out' technique, which is highlighted by releasing the posterolateral capsule in valgus knees (posteromedial in varus) followed by pie crusting of the iliotibial band (or superficial MCL). After a rectangular extension gap is achieved, the femur is appropriately sized to restore the posterior condylar offset.
Next, attention is turned to creating an equal and rectangular flexion-gap via the 'parallel to the tibial cut technique'. By this technique a cutting block is attached to the distal femur and a laminar spreader is used to tension the knee. Then the posterior femur is resected creating an equal and rectangular flexion-gap (~18-20 mm) which ideally is slightly smaller than the extension gap.
Trial components are then used to assess the stability of the joint. Once satisfied with stability of the joint the final components are cemented into place using good cementation technique. Prior to the insertion and final reduction of the liner, the posterior capsule and posteromedial and posterolateral structures are injected with the first periarticular injection. A second injection is performed into the synovium, capsule, extensor mechanism, iliotibial band, collateral ligaments and the anteromedial capsule following insertion of the liner and final reduction. Finally the knee is ranged and assessed for final stability.
Results
Our institution has had excellent clinical results using these gap-balancing and pain management techniques [1, 3, 7]. We have found that extension-first balancing followed by the 'parallel to the tibial cut technique' accurately restores rotational alignment better than using bony landmarks [2]. Improved alignment has also translated into excellent clinical outcomes in both the short- and long-term [1, 3, 7], as well as excellent long-term survivorship. In fact, using these techniques in a posterior-stabilized design, we have found 100% survivorship for mechanical failure and 98% for any revision, at ten-year follow-up [7].
We have also performed several studies focusing on this multimodal pain protocol, highlighted by the addition of corticosteroid in the peri-articular injection. We have found that this technique provides low manipulation rates, better pain control, lower narcotic use, reduced hospital stay, and earlier functional recovery [6, 8]. Despite some reports that corticosteroid use may increase the risk of infection, a recent unpublished review of all primary TKAs performed by us between the years of 2008 and 2013 (536) showed that two cases only required reoperation for a superficial or deep joint infection. This pain protocol has proven to be an effective means of providing pain management and improving outcomes after TKA.
Conclusions
Appropriate soft-tissue balancing and pain control are important components to providing a successful TKA. Through the extension-first balancing using the 'inside-out' and 'parallel to the tibial cut' techniques we have had excellent clinical results. Coupled with a multimodal pain protocol, we have found a highly successful approach to performing primary TKAs.
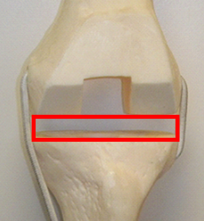 | Balance the extension-gap first, using soft-tissue balancing. When necessary the 'inside-out technique' can be used to correct moderate-to-severe deformities. The releases start by (1) completely resecting the PCL, (2) releasing the posterolateral capsule (in a valgus deformity) up the posterior border of the iliotibial band at the level of the tibial cut in extension (see image), (3) iliotibial band is pie-crusted. |
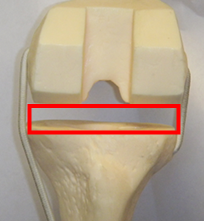 | Balance flexion-gap after balancing the extension gap using the 'parallel to the tibial cut technique'. Once the tibia has been cut perpendicular to its long axis, the femur should be cut parallel to the tibial cut. |
References:
- Meftah M, Blum YC, Raja D, Ranawat AS, Ranawat CS. Correcting fixed varus deformity with flexion contracture during total knee arthroplasty: the "inside-out" technique: AAOS exhibit selection. J Bone Joint Surg Am. 2012 May 16;94(10):e66.
- Vaidya SV, Gadhiya RM, Bagaria V, Ranawat AS, Ranawat CS.Computed tomographic evaluation of femoral component rotation in total knee arthroplasty.Indian J Orthop. 2013 Jan;47(1):40-4
- Ranawat AS, Ranawat CS, Elkus M, Rasquinha VJ, Rossi R, Babhulkar S. Total knee arthroplasty for severe valgus deformity. J Bone Joint Surg Am. 2005 Sep;87Suppl 1(Pt 2):271-84.
- Meftah M, Wong AC, Nawabi DH, Yun RJ, Ranawat AS, Ranawat CS. Pain management after total knee arthroplasty using a multimodal approach. Orthopedics. 2012 May;35(5):e660-4.
- Maheshwari AV, Blum YC, Shekhar L, Ranawat AS, Ranawat CS. Multimodal pain management after total hip and knee arthroplasty at the Ranawat Orthopaedic Center. ClinOrthopRelat Res. 2009 Jun;467(6):1418-23.
- Parvataneni HK, Shah VP, Howard H, Cole N, Ranawat AS, Ranawat CS. Controlling pain after total hip and knee arthroplasty using a multimodal protocol with local periarticular injections: a prospective randomized study. J Arthroplasty. 2007 Sep;22(6 Suppl 2):33-8. Epub 2007 Jul 26.
- Meftah M, Ranawat AS, Ranawat CS. Ten-year follow-up of a rotating-platform, posterior-stabilized total knee arthroplasty. J Bone Joint Surg Am. 2012 Mar 7;94(5):426-32.
- Sharma V, Maheshwari AV, Tsailas PG, Ranawat AS, Ranawat CS.The results of knee manipulation for stiffness after total knee arthroplasty with or without an intra-articular steroid injection.Indian J Orthop. 2008 Jul;42(3):314-8.


















