SICOT Global Network for Electronic Learning - SIGNEL
Case of the Month
Newsletter Editorial Board Member - Minsk, Belarus
Patient History
A 25-year-old male patient involved in a road traffic accident sustained multiple injuries as follows:
Closed-head injury, concussion of the brain, chest contusion, bilateral displaced fractures of the pubic and ischial bones alongside injury to the left and right sacroiliac joints, open comminuted fracture of the right femur, open comminuted fractures of the right 4th and 5th metacarpals and multiple lacerations.
Damage control (DC) on admission was performed. A 3D CT image after DC-surgery is provided below:

Q1: When would you do the second stage? What is your plan of management?
In 14 days, definitive surgery was performed: ORIF for the pelvis and IM-nailing of the femur.


The patient was discharged in satisfactory condition and started rehabilitation.
He returned 6 months later… There were no complaints regarding the pelvis, head and chest, but he had pain in the right femur. He had redness and induration over the medial aspect of the middle third of his right thigh (far away from the surgical incisions). The right thigh was significantly swollen compared to the left thigh. There were no open wounds or fistulae. СRP was 233 mg/l, ESR 89 mm/h, WBC 13.4*10^9/l.


Q2: What is the problem now? What should we do?
Clearly, the patient has developed late infection after the IM-nailing. However, we decided to perform an MRI scan to evaluate the soft tissue swelling around the mid-thigh region as we were worried that a simple debridement +/- exchanging of the nail may be inadequate.
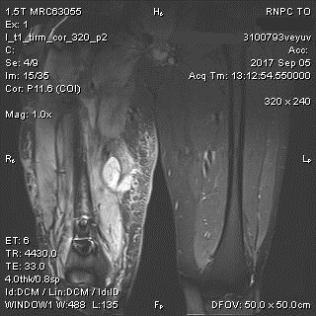

The MRI confirmed the presence of an abscess at the area of concern.
Q3: What management options do we have?
We removed the nail, performed thorough debridement of the IM canal and soft tissues around the surgical wounds and incised and drained the abscess in the mid-thigh through a separate incision. Intraoperative specimens were sent for microbiology assessment. Two microorganisms were grown: Staphylococcus aureus and Enterobacter cloacae. Two weeks later, the fracture was fixed with a nail coated with gentamycin and meropenem loaded cement according to the sensitivity results.


Two years later, the patient is fully weight-bearing without any complaints. He required one more surgery for nail dynamisation, but the infection has not recurred.
Discussion
Successful management of long bone osteomyelitis is a challenge both for the surgeon and the patient. Magnetic resonance imaging (MRI) is the best choice to evaluate soft-tissues and gives additional information about intramedullary infection [1]. A number of authors state that metal artefacts can impair correct evaluation postoperatively in the presence of metalwork and scarring or oedema associated with bony defects may mimic infection [2,3]. However, in this case (and it is not unique), we see that MRI can provide very useful information and in fact, changed our management strategy.
- Kleber C, Schaser KD, Trampuz A. Complication management of infected osteosynthesis: therapy algorithm for peri-implant infections. Chirurg 2015; 86:925–34.
- Metsemakers W. J. et al. Infection after fracture fixation: current surgical and microbiological concepts. Injury 2018; 49(3):511-522.
- Ledermann HP, Kaim A, Bongartz G, Steinbrich W. Pitfalls and limitations of magnetic resonance imaging in chronic posttraumatic osteomyelitis. Eur Radiol 2000; 10:1815–23.





















