Expert Corner
How I do a Medial Patello-Femoral Ligament (MPFL) Reconstruction for Recurrent Patella Instability
 Gandhi Nathan Solayar Gandhi Nathan SolayarSeremban, Malaysia |
Introduction
Recurrent patella instability may stem from a multitude of various factors. It is important for the surgeon to recognise that one solution may not fit all presentations. There are over a hundred different surgical methods described covering a range of bony to soft tissue procedures to address this issue [1].
Pre-operative
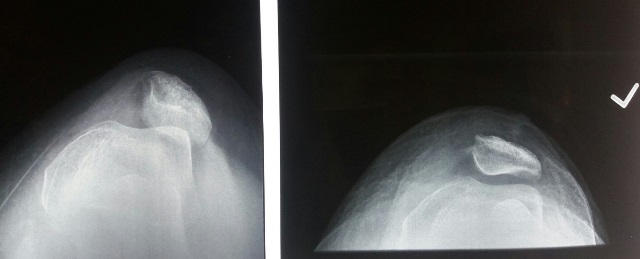
I begin with careful patient selection as this is key in choosing the right operation. Detailed history is important to elucidate underlying connective tissue disorders and prior surgery to the affected knee among other things. Clinically, I assess the degree of apprehension, reducibility, patella tilt and carefully document any prior surgical scars. I always document the patient’s gait and look for excessive valgus on stance. My standard radiographs which I request for every patient include bilateral weight-bearing AP and lateral radiographs. This is important to check for excessive knee valgus as I believe that an MPFL would not suffice without first addressing the valgus angulature. I always request a patella skyline view at 30° flexion to allow for assessment of the degree of patella tilt which I use to decide whether a lateral patella retinacular release is required.
I routinely get MRIs for all knees prior to undergoing surgery for a few reasons. Firstly, I determine the tibial tubercle-trochlear groove (TT-TG) distance and document this. My cut off for most patients is 18mm and if it were more than this, I would include a tuberosity realignment procedure (I prefer to do a Fulkerson’s osteotomy in these cases). An MRI also allows for accurate measurements of patella alta (I use the Insall-Salvati ratio) and if it is more than 1.5, I would perform a distalization of the tibial tuberosity. Finally, I document the trochlear sulcus angle (deepest part of the groove on the axial view). If this is flat (or in rare instances, a positive angle) a sulcus deepening procedure such as a V-osteotomy would be an option.
Surgery
After consenting the patient and explaining the procedure, I request for a general anaesthesia for my MPFL cases (to allow for immediate knee mobilisation post procedure as opposed to a spinal anaesthetic). I routinely use a tourniquet and have a foot positioner having the knee at 30° flexion. I perform an examination under anaesthesia (EUA) in every case, documenting the degree of lateral patella translation and patella tracking.
I first start with a routine diagnostic arthroscopy, paying special attention to the trochlear and patella chondral surfaces. In cases with chondral tears, I debride the defect to a stable rim and I prefer using radio-frequency ablation (RFA) arthroscopically to stabilise any frayed chondral surfaces. In my experience, I perform a lateral retinacular release if there is evidence of significant patella tilt on the skyline radiographs or if I am unable to clinically translate the patella sufficiently medial during my EUA. I perform this release arthroscopically using RFA about a centimetre off along the full lateral border of the patella till I visualise the fibres of vastus lateralis thus ensuring adequate release. After this release, I translate the patella medially and observe the patella tracking arthroscopically to ensure adequate patella mobilisation.
The next stage would be harvesting the hamstrings. I prefer semi-tendinosis autografts for all my MPFLs. I believe the semi-tendinosis graft alone is sufficient and I tend to leave the gracilis intact. One technique I do is to secure each graft end with different colour sutures as this helps in determining specific tensioning of each graft end. I size the double-folded graft, pre-tension them at 15lbs and cover it in a vancomycin soaked gauze.
I then proceed to perform a mid-line incision over the patella and develop skin flaps medially. I dissect sub-periosteally down the patella medially as this makes it easy to identify the space between retinaculum and capsule without piercing the joint. In my hands, I prefer an “on-lay” technique instead of drill holes in the patella for a few reasons. Drilling holes results in stress risers and increases the risk of patella fractures. I can always resort to drilling if my suture anchors fail intra-op and, therefore, I keep this option as a last resort. With the medial side of patella exposed, I create a 3mm groove with a rongeur (from the supero-medial corner to about halfway down the patella) (Figure 1). I then place 2 x suture anchors (I have been using the 2.9mm Juggerknot™ anchors) with about a 1cm space in between them. Then, with my assistant keeping adequate tension, I secure the mid-portion of the graft to the patella keeping sure that the graft is well embedded in the groove just fashioned. Further spot-weld points of fixation may be added later at the end of the case by suturing some parts of the graft to the patella periosteum and retinaculum.
I then proceed to identify the insertion point on the medial femur. I normally do this radiologically to identify the isometric point. This point lies just above the confluence of lines connecting Blumensaat’s and the posterior femoral cortex [2]. I insert a guide pin with an eyelet from that point, aiming anteriorly and superiorly to exit the lateral cortex without inadvertently crossing through the knee joint. Through a small stab incision (less than 1cm), I debride the medial cortex and ream a tunnel to correspond to the graft size (I ream right across the femur but just before the lateral cortex). Then, I develop a plane between the medial retinaculum and capsule from the patella down to the entry point of my pin, feed a shuttling suture through and pass my graft between the two layers. Finally, the graft is passed through the medial femoral cortex using the guide pin and the suture ends on the lateral side can be tensioned independently (using the different colour sutures mentioned earlier). I cycle the knee a few times and use a bio-absorbable interference screw 1mm larger than the reamed tunnel. I secure the MPFL graft with the knee in about 30° of flexion and ensure that the patella is clinically able to translate halfway across the trochlear in extension to avoid over-tensioning. I routinely assess patella tracking arthroscopically after every MPFL reconstruction and use a knee brace post-operatively allowing for movement from 0 to 90° of flexion.
Postoperatively, I allow full weight-bearing with crutches and refer all patients for quadriceps strengthening physiotherapy with an emphasis on the vastus medialis oblique (VMO). I generally limit my patients to 90 degrees of flexion for 6 weeks before proceeding to full range of motion. However, this is done on a case-to-case basis with consultation from my sports rehabilitation physicians at my centre. Full return to sporting activities is normally achieved at between 4 and 6 months post-operatively.
- Li J, Li Y, Wei J, Wang J, Gao S, Shen Y. A simple technique for reconstruction of medial patellofemoral ligament with bone-fascia tunnel fixation at the medial margin of the patella: a 6-year-minimum follow-up study. J Orthop Surg Res [Internet]. 2014 Aug 15 9(1):66.
- Trinh TQ, Ferrel JR, Bentley JC, Steensen RN. The Anatomy of the Medial Patellofemoral Ligament. Orthopedics [Internet]. 2017 Jul 1;40(4):e583–8.


















