
SICOT Global Network for Electronic Learning - SIGNEL
Case of the Month
Management of Osteolysis and Component Loosening in a Hybrid Total Hip Replacement
Affiliations:
- Clinical Orthopaedic Surgery Fellow, Hospital for Special Surgery, New York, NY, USA
- Assistant Attending Orthopaedic Surgeon, Hospital for Special Surgery, New York, NY, USA
Case Presentation
A 56-year-old gentleman, who had undergone a left total hip arthroplasty (THA) eighteen years ago for failed slipped capital femoral epiphysis (SCFE) pinning, presented with increasing pain in his left hip and thigh over the last three years. He had a significant decline in his function over the last year. He ambulated with crutches and was unable to bear weight on the left leg. He had become essentially immobile from his condition. He denied fevers or chills and had no rest or night pain. He took narcotic analgesics for pain control daily.
His past medical history was significant for hypertension and insulin-dependent diabetes mellitus, complicated by bilateral lower extremity neuropathy and stage IV chronic kidney disease. His medications included anti-hypertensives, oral anti-hyperglycemics and insulin, and gabapentin. He had no allergies. He denied smoking and rarely consumed alcohol.
On physical examination, the patient was 193 cm tall and weighed 117 kg (body mass index, 32 kg/m²). He was unable to walk without crutches. Stinchfield testing was negative, but he had severe pain with hip rotation. He had hip flexion of 90 degrees, external rotation of 50 degrees, internal rotation of 5 degrees, abduction of 30 degrees, and adduction of 10 degrees. He had normal power distally in the left leg and foot. His sensation to light touch was diminished distal to the knee. The skin was intact, warm and well-perfused distally, but there were no palpable pulses.
Standard plain radiographs (Figure 1A-C) demonstrated a hybrid left THA. Prior radiographs were reviewed for comparison. There was severe, progressive osteolysis around the femoral component, with a chronic osteolytic fracture of the greater trochanter. There was a cortical breach at the tip of the femoral stem posterolaterally, and femoral component migration indicative of loosening. There was eccentric polyethylene liner wear.
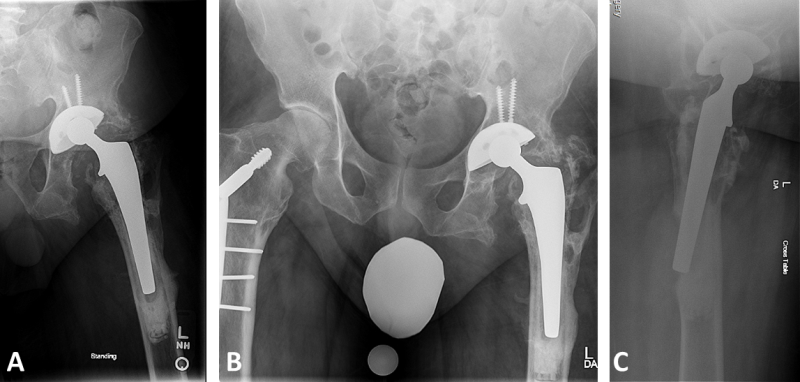
Figure 1
What are your next steps in management?
An infection work-up was performed. C-reactive protein (CRP) was 0.9 mg/dL (normal), erythrocyte sedimentation rate (ESR) was 38 mm/hour (elevated), and serum white blood cell (WBC) count was 4.8 per nL (normal). The serologic results were considered somewhat equivocal. Therefore, an aspiration was performed, returning 125 WBC cells/mm³ and negative cultures. His hemoglobin A1C was 5.54%, indicating good glycemic control.
Additional cross-sectional imaging (computed tomography) was performed to assess the extent of both femoral and acetabular osteolysis (Figure 2A-C). Retroacetabular osteolysis was present, but there appeared to be spot-welds of trabecular bone. Acetabular orientation was 10 degrees of anteversion and 35 degrees of abduction, and there was 25 degrees of femoral component retroversion.
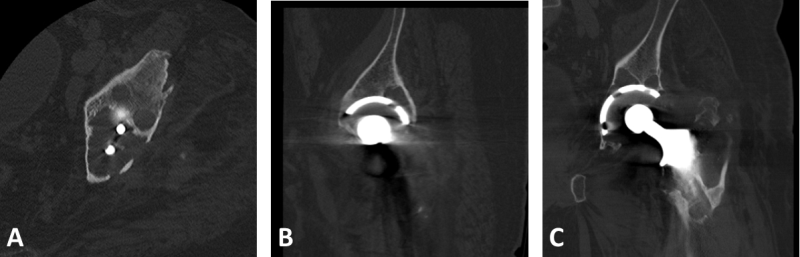
Figure 2
What is your treatment plan for this patient?
Revision of both components
Femoral revision with head/liner exchange and bone grafting
Isolated acetabular revision and bone grafting
Head/liner exchange with bone grafting only
Two-stage exchange arthroplasty
Although femoral component perforation may not adversely affect the mid-term results of cemented femoral components [1], the progressive migration of the femoral component on serial radiographs indicates that the stem was loose. The stability of the acetabular component was not definitive on imaging. Therefore, the patient was listed for revision of his left femoral component, with the understanding that his acetabular component would be evaluated intra-operatively for stability and possible revision.
An extensile posterolateral approach to the hip was performed. The vastus lateralis was elevated anteriorly, exposing the approximately 2 cm cortical defect with the protruding stem and exposed distal cement mantle. In order to access the proximal and distal cement mantle, an osteotomy was performed, extending from the 2 cm defect proximally, posteriorly, and anteriorly. The separate greater trochanteric piece was retained in a continuous soft tissue sleeve between the abductor musculature and the vastus lateralis. The femoral component was grossly loose and easily removed. The remaining cement mantle was then removed with a combination of curved osteotomes and ultrasonic tools. A prophylactic cable was passed distal to the osteotomy and the femoral canal was prepared to accept a modular, fluted, tapered stem (Restoration Modular, Stryker Corp., Kalamazoo, MI, USA). For the femoral reconstruction a 26 mm x 235 mm conical stem was required for adequate distal cortical fixation and to bypass the cortical defect by at least 2 cortical widths. A + 30 mm proximal body was required to restore leg length.
Attention was then turned to the acetabulum. The acetabulum was exposed, and the liner was removed. The two acetabular screws were removed, and the acetabulum was checked for stability and found to be well fixed to the pelvis. Due to the size of the implanted acetabular shell (62 mm) and the fact that it was well-fixed, the decision was made to retain it and place bone graft into the areas of acetabular osteolysis. Evidence suggests that cup retention and bone grafting has a high likelihood of success [2]. However, there was concern for abductor insufficiency in the setting of greater trochanteric non-union [3], and there is generally a greater risk for prosthetic dislocation after revision THA compared to primary THA [4]. Therefore, additional constraint was desired. However, a fully constrained liner was not used, since it may have a higher risk for failure given the patient’s young age, weight, and goals for activity [5]. Dual mobility components have been shown to reduce the prevalence of hip instability after revision THA [6]. A double-socket technique has been described to preserve acetabular bone stock and convert bearing couples for revision THA [7]. A 52 mm dual mobility shell (ADM X3 Mobile Bearing Hip System, Stryker Corp., Kalamazoo, MI, USA), which articulates with a 46 mm polyethylene bearing, was cemented into the retained component allowing for a 2 mm cement mantle. The ADM shell has a roughened HA coating with peripheral ridges which permits better cement inter-digitation and fixation compared to the cobalt chrome liner from the modular dual mobility (MDM) acetabular system (Stryker Corp., Kalamazoo, MI, USA). The dual mobility shell was cemented in increased anteversion compared to the retained shell, which was under-anteverted based on preoperative imaging and intraoperative assessments. The final femoral component was then implanted, correcting femoral version and restoring leg length and offset (Figure 3A-B).
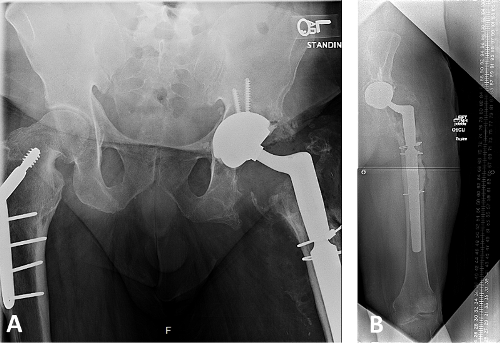
Figure 3
The osteotomy was repaired using cables. The greater trochanter fracture was not fixed, given its chronicity and stability of the fragment within its soft tissue sleeve. Closure proceeded in layers. The patient was instructed to maintain toe-touch weight-bearing for 6 weeks postoperatively, at which point he was progressed to full weight-bearing. At 3 months the patient was doing well, with full weight-bearing and without complication.
Take Home Points
Cortical perforation is not an indication for femoral revision, in the setting of cemented femoral fixation [1].
Progressive component migration on serial radiographs indicates that a component is loose.
Retention of a well-fixed cup and bone grafting in the setting of acetabular osteolysis is an acceptable option, with a good probability of success [2]; Cup retention avoids the need for complex acetabular reconstruction in the setting of massive acetabular bone loss.
Revision THA and abductor insufficiency increase the risk for postoperative prosthetic dislocation [3,4].
Constrained acetabular liners and dual mobility bearings can reduce the risk of dislocation [5,6], but fully constrained liners may be less suitable for young, active patients.
A “double-socket” technique is useful in the setting of large, stable acetabular shells, for which conversion of the bearing couple is desirable [7]; In this case, a dual mobility acetabular shell was cemented into the retained cup, permitting implantation of large “effective head” polyethylene articulation.
- Pellicci PM, Inglis AE, Salvati EA. Perforation of the femoral shaft during total hip replacement. J Bone Joint Surg Am. 1980 Mar;62(2):234-40.
- Maloney WJ, Herzwurm P, Paprosky W, Rubash HE, Engh CA. Treatment of pelvic osteolysis associated with a stable acetabular component inserted without cement as part of a total hip replacement. J Bone Joint Surg Am. 1997 Nov;79(11):1628-34.
- Wera GD, Ting NT, Moric M, Paprosky WG, Sporer SM, Della Valle CJ. Classification and management of the unstable total hip arthroplasty. J Arthroplasty. 2012 May;27(5):710-5.
- Wetters NG, Murray TG, Moric M, Sporer SM, Paprosky WG, Della Valle CJ. Risk factors for dislocation after revision total hip arthroplasty. Clin Orthop Relat Res. 2013 Feb;471(2):410-6.
- Noble PC, Durrani SK, Usrey MM, Mathis KB, Bardakos NV. Constrained cups appear incapable of meeting the demands of revision THA. Clin Orthop Relat Res. 2012 Jul;470(7):1907-16.
- Philippot R, Adam P, Reckhaus M, Delangle F, Verdot F, Curvale G, Farizon F. Prevention of dislocation in total hip revision surgery using a dual mobility design. Orthop Traumatol Surg Res. 2009 Oct;95(6):407-13.
- Beaulé PE, Ebramzadeh E, Le Duff M, Prasad R, Amstutz HC. Cementing a liner into a stable cementless acetabular shell: the double-socket technique. J Bone Joint Surg Am. 2004 May;86-A(5):929-34.

















