
SICOT Global Network for Electronic Learning - SIGNEL
Case of the Month
Treating Chronic Arthrofibrosis After Primary Total Knee Arthroplasty
²Assistant Attending Orthopaedic Surgeon, Hospital for Special Surgery, New York, NY, USA
Case Presentation:
A 67-year-old woman presented 6 years after right primary total knee arthroplasty (TKA) with a complaint of severe knee stiffness, reduced range of motion (ROM), and pain. The TKA had been performed at an outside institution. Immediately after her primary surgery, her wound healed uneventfully, but she never achieved significant improvements in her ROM postoperatively. She had failed early manipulations under anesthesia (MUA) as well as arthroscopic lysis of adhesions. She had pain which bothered her at night, she had great difficulty with stairs and with performing basic activities of daily living. She ambulated with a cane. She could not tolerate anti-inflammatories because of her history of ulcerative colitis. She denied fevers and chills.
Her past medical history was significant for ulcerative colitis, hypertension, and hypercholesterolemia. She was currently taking infliximab, simvastatin, valsartan, and balsalazide.
On physical examination she was an overweight woman in no acute distress. She ambulated with a limp. Her wound was well-healed. There was no appreciable warmth or erythema. There was no appreciable effusion, but there was a palpable, firm scar anterior to the knee. She had a 5-degree knee flexion contracture, and achieved knee flexion to 25 degrees only. There was no instability in any plane. Her neurovascular exam of the extremity was normal.
Radiographic examination (Figure 1A-C) showed well-fixed and well-aligned implants, with slight lateral patellar tilt on the merchant view. The posterior condylar offset appeared appropriate, and the implants did not appear oversized.
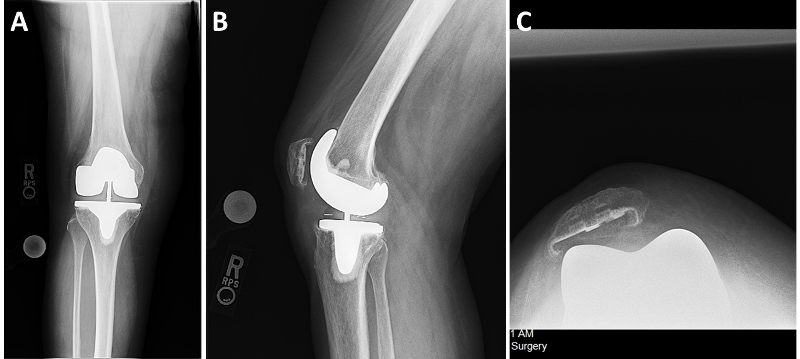
Fig. 1
What are your next steps in management?
Although the patient had no other localizing signs for infection, she underwent further serological testing for infection. Her white blood cell count was 6.8, C-reactive protein and erythrocyte sedimentation rate were within normal ranges. Therefore, there was a low suspicion for peri-prosthetic joint infection.
Which of the following would be your next step for treating this patient?
Physical therapy
MUA
Revision TKA
Arthroscopic lysis of adhesions (LOA)
Open LOA
The patient was counselled that there were few treatment options left that could reliably restore ROM to her knee. She was offered revision TKA as a final solution to her problem [1].
Her prior anterior midline incision was utilized, and an extended medial parapatellar arthrotomy was sufficient for exposure. Extensive scar was excised from the suprapatellar pouch, medial and lateral gutters, and infrapatellar region. As part of the exposure, a full soft tissue “peel” of the distal femur was performed, releasing the collateral ligaments and the posterior soft tissue envelope. Care was taken to elevate the femoral origins of the collateral ligaments in continuous soft tissue sleeves in order to permit their scarring down in continuity to bone. Both the femoral and tibial components were removed. To ensure full knee extension a liberal fresh cut of the distal femur was performed. A hinged construct (S-ROM Noiles, Depuy Synthes, Warsaw, IN, USA) was implanted using hybrid fixation, including porous sleeves in the metaphyses, uncemented stems in the diaphyses, and bone cement at the interfaces between the bone, tibial baseplate and femoral resurfacing component. The quadriceps was scarred anteriorly to the femur, and was elevated to improve extensor mechanism excursion. A full release of the lateral retinaculum was performed to optimize patella tracking. The prior patellar resurfacing component was well-fixed and was retained. The wound was closed in layers over a deep drain, which was maintained for 24 hours postoperatively. The final intraoperative ROM was slight recurvatum to 120 degrees of flexion. She was permitted full weight-bearing, and postoperative physical rehabilitation was directed at maintaining knee extension and maximizing knee flexion. Continuous passive motion was not used. Coumadin was used as prophylaxis for venous thromboembolism.
What other measures would you take to enhance the odds for treatment success in this patient?
No adjuvant treatments for arthrofibrosis have been studied rigorously. However, it has been recognized that the histopathology for arthrofibrosis closely mimics that of heterotopic ossification, and there are microscopic foci of HO in tissue specimens from some cases of arthrofibrosis [2,3]. Radiation is commonly used to prevent the recurrence of HO [3], and thus there may be rationale for using radiation to prevent arthrofibrosis [1]. Anecdotally we have observed reliable success with this treatment protocol.
In this patient, we used single-dose postoperative radiation to prevent recurrence of arthrofibrosis. At four weeks postoperatively, her wound had healed. She achieved full knee extension and flexion to 90 degrees. Her radiographs show excellent alignment in the coronal plane and improved patellar tracking (Figure 2A-D).
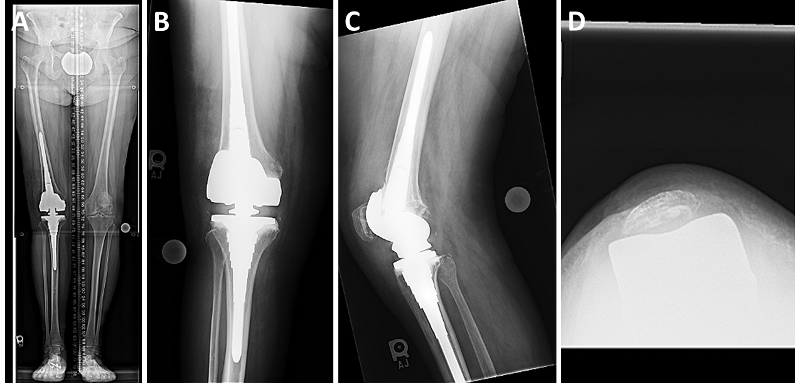
Fig. 2
Take Home Points:
Arthrofibrosis is a challenging problem after TKA
Late MUA and lysis of adhesions are unlikely to improve ROM
Revision TKA with a hinged component permits full release of the scarred soft structures and femoral shortening, maximizing ROM [1]
Releasing collateral ligaments in continuous soft tissue sleeves may permit their scarring down in continuity to bone
Perform bone cuts to ensure full extension, erring toward leaving the knee “loose”
The histopathology of arthrofibrosis frequently contains foci of heterotopic ossification, the presence of which correlates with decreased ROM [2]
Adjuvant radiation may prevent recurrence of arthrofibrosis [1,3]
- Farid YR, Thakral R, Finn HA. Low-dose irradiation and constrained revision for severe, idiopathic, arthrofibrosis following total knee arthroplasty. J Arthroplasty. 2013 Sep;28(8):1314-20.
- Freeman TA, Parvizi J, Dela Valle CJ, Steinbeck MJ. Mast cells and hypoxia drive tissue metaplasia and heterotopic ossification in idiopathic arthrofibrosis after total knee arthroplasty. Fibrogenesis Tissue Repair. 2010 Sep 1;3:17.
- Ranganathan K, Loder S, Agarwal S, Wong VW, Forsberg J, Davis TA, Wang S, James AW, Levi B. Heterotopic Ossification: Basic-Science Principles and Clinical Correlates. J Bone Joint Surg Am. 2015 Jul 1;97(13):1101-11.

















