SICOT Global Network for Electronic Learning - SIGNEL
Case of the Month
History
A 20-year-old female presented with right knee pain and swelling over one month. The swelling has progressively worsened over that period. Patient denied any history of recent trauma or sport injuries. She also denied any febrile episode. She had no history of surgery to the right knee. She denies any weight loss or night pain.
On examination, she was walking with an antalgic gait. Knee effusion was clinically detected. No focal bony tenderness. Knee range of motion was slightly restricted. The knee was grossly stable. Radiograph of right knee was performed.
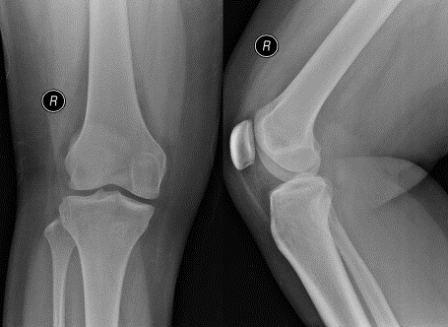
Q. What are your thoughts on the findings of the knee radiograph?
Normal bony contour. No fracture noted. Raised suprapatellar fat pad suggesting intra-articular knee effusion.
Q. What is the next step in your management plan?
Inflammatory markers (FBC/ESR/CRP/Uric acid/Rheumatoid Factor)
Joint aspiration for C+S/microscopy for crystal
MRI scan of the knee
All of the above
Her CRP and ESR were raised. WBC, Uric acid and rheumatoid factor were normal.
Joint aspiration showed bloody coloured synovial fluid. No crystal or organism seen on microscopy. Gram stain was negative.
MRI of the knee was performed.

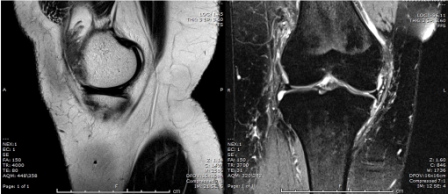
Q. What is your opinion on the MRI scan?
Knee joint effusion
Hypertrophy of the synovium
Normal cartilage and bony outline. Meniscus, ACL, and PCL were intact.
Q. What is your next plan of management?
A diagnostic knee arthroscopy and biopsy was performed. This is the arthroscopic view during arthroscopy.
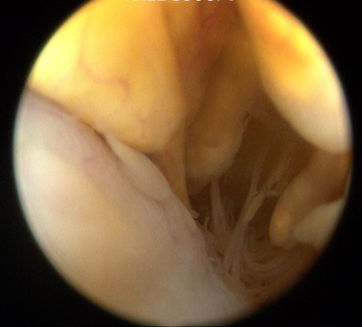
Q. What is your diagnosis?
Diagnosis: Pigmented villonodular synovitis
Pigmented villonodular synovitis (PVNS) is a rare benign proliferative condition affecting synovial membranes of joints, bursae or tendons, resulting from possibly neoplastic synovial proliferation with villous and nodular projections and haemosiderin deposition. PVNS is most commonly mono articular (80% knee joint) but occasionally it can be oligo articular [1].
The histology of PVNS can look similar to some aggressive neoplasms (rhabdomyosarcoma, synovial sarcoma, epithelioid sarcoma) and imaging therefore has an important role for definitive diagnosis [2].
Clinical presentation is pain with joint effusion, which is usually chronic and slowly progressive. Diagnosis could be delayed for months before patient presented [1].
Radiographs likely show non-specific features such as joint effusion and bone erosions. CT and ultrasound can also demonstrate the hypertrophic synovium as a slightly hyperdense/echogenic soft tissue mass. Bony erosion can be seen well on CT scan [4].
MRI is the best approach showing the masslike synovial proliferation with lobulated margins, with low signal intensity and "blooming" artifact on gradient echo due to haemosiderin deposition [4].
PVNS can be classified into localised or diffuse form. The localised form is usually extra articular and the diffuse form is usually intra articular [1].
Complete synovectomy is the treatment of choice. Complete synovectomy of the knee joint can be performed either through an open or arthroscopic approach. Complications such as high recurrence rate from arthroscopic synovectomy and joint stiffness from open procedure has been reported. Adjuvant radiotherapy has been shown to be effective in reducing the risk of recurrence [5].
References:
- Tyler WK, Vidal AF, Williams RJ et al. Pigmented villonodular synovitis. J Am Acad Orthop Surg. 2006;14:376–85.
- Barile A, Sabatini M, Iannessi F et al. Pigmented villonodular synovitis (PVNS) of the knee joint: magnetic resonance imaging (MRI) using standard and dynamic paramagnetic contrast media. Report of 52 cases surgically and histologically controlled. Radiol Med. 2004;107(4):356-66
- Kramer DE, Frassica FJ, Frassica DA et al. Pigmented villonodular synovitis of the knee: diagnosis and treatment. J Knee Surg. 2009;22:243–54
- Bravo SM, Winalski CS, Weissman BN. Pigmented villonodular synovitis. Radiol. Clin. North Am. 1996;34 (2): 311-26
- Nasser WAM, Bassiony AA, Elghazaly HA. Treatment of Diffuse Pigmented Villonodular Synovitis of the knee with combined surgical and radio synovectomy. HSS J. 2009;5(1): 19-23


















