SICOT Global Network for Electronic Learning - SIGNEL
Case of the Month
October 2014
Authors: John Mukhopadhaya, A.A. Hai, & Shalin MaheshwariHistory
38-year-old male patient presents with pain in the left groin and thigh in the past four years. The pain has increased in intensity in the past month and inability to walk in the past four days. On examination, the patient had tenderness over left groin and trochanter. Range of motion at hip was painful and restricted. Patient had normal distal neurovascular status without any other co-morbidities.

Fig. 1 â X-ray of pelvis with both hips with femur AP view

Fig. 2 â X-ray of skull â lateral view showing multiple lytic areas
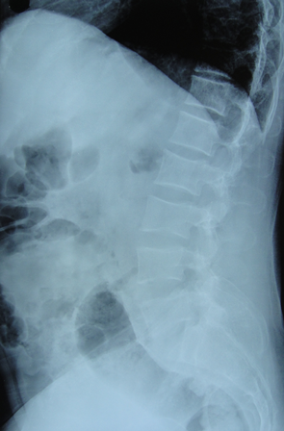

Fig. 3 â Lumbar spine AP and lateral showed osteoporotic changes
Investigations revealed severely elevated Serum Calcium (13.2 mg/dl), elevated Se. Alkaline Phosphatase and low Se. Phosphorous, markedly elevated Parathyroid hormone levels, low Vitamin D3 levels and normal renal profile.
What is your provisional diagnosis for this patient?
Diagnosis
Pathological fracture of the left proximal femur of unknown aetiology.
What would be your next step in the management of this patient?
- Immediate Internal Fixation
- Further investigate in form of Bone Scan/MRI/CT Scan/Biopsy/Hormonal Profile
- Observe under Conservative Treatment
The patient was investigated in the form of a Bone Scan which revealed multiple hot spots in the skull, ribs, dorsal and lumbar spine, pelvis, and left femur. Bone scan also showed multiple active areas in neck around thyroid gland. Further ultrasound examination revealed hypoechoeic, hypervascular cystic areas bilateral parathyroid regions. This was collaborated with markedly elevated Parathyroid Hormone levels and presence of urinary calculi making it a case of Primary Hyperparathyroidism.
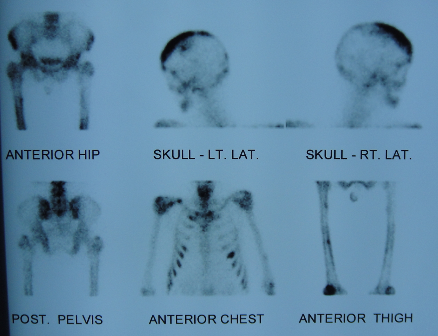
Fig. 4 â Bone Scan image showing global hot spots
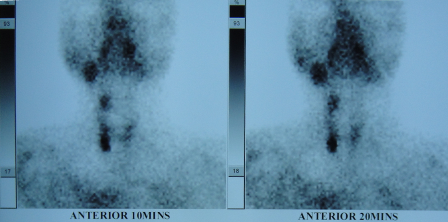
Fig. 5 â Specific Thyroid Scan showing active areas in parathyroid gland
How will you manage this further?
- Proceed with Internal Fixation of the Left Proximal Femur
- Removal of Parathyroid gland and then proceed with Internal Fixation of the Left Proximal Femur
- Conservative treatment
Parathyroid glands were explored and removed by a general surgeon and biopsy confirmed it to be Parathyroid adenoma. The patientâs Serum Calcium levels normalised rapidly to normal levels within a weekâs time. Increased pain during this perioperative period showed complete fracture and he was then taken up for fixation of the fracture in ipsilateral neck and subtrochanteric region with supracondylar locking plate by minimally invasive technique. Post-op patient was kept non weight bearing for 6 weeks and blood profile monitored for Calcium, PTH levels. Radiologically, he showed gradual improvement and was allowed complete weight bearing after 8 weeks.
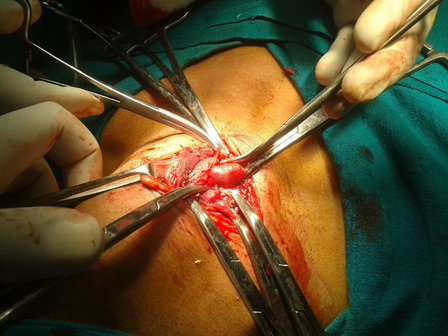
Fig. 6 â Intra-op image of adenoma

Fig. 7 â Removed parathyroid adenoma
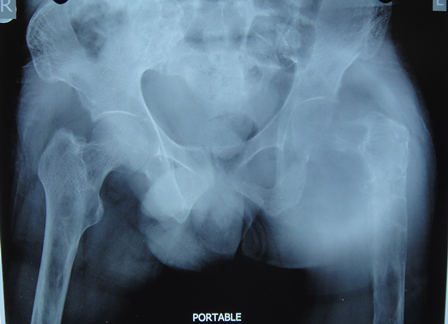
Fig. 8 â Complete fracture during peri-op period
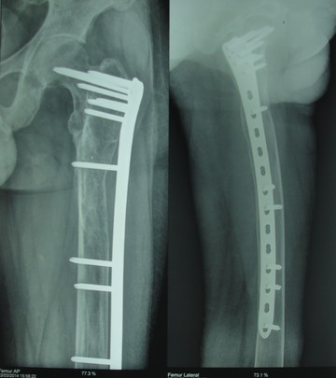
Fig. 9 â Follow-up X-ray at 6 months
 Â
 
Fig. 10 â Clinical function at 6 months
Discussion
Hyperparathyroidism commonly presents with symptoms of hypercalcaemia such as abdominal pain, bone pain, fatigue, depression and nephrolithiasis. It can be classified into three main groups. Primary hyperparathyroidism is due to parathyroid adenoma in 85% of patients, the remainder are due to multiple adenomas and parathyroid cancers. It affects 1 in 2,000 men annually [1]. Secondary hyperparathyroidism is due to chronic vitamin D deficiency as a result of chronic renal failure. Tertiary hyperparathyroidism is a result of autonomous parathyroid stimulation following a period of persistent parathyroid stimulation. Biochemical investigations reveal raised calcium, raised PTH and decrease in phosphate levels in the blood.
The use of preoperative localisation studies is controversial. Main methods of imaging are ultrasound, computed tomography and nuclear imaging. Technetium Tc 99 m sestamibi is the radio-pharmacological agent of choice, with a sensitivity reported to be between 72%-100% [2]. A recent study has shown that sestamibi combined with ultrasound increases the accuracy of detection for parathyroid adenomas [3].
The use of preoperative localisation studies is controversial. Main methods of imaging are ultrasound, computed tomography and nuclear imaging. Technetium Tc 99 m sestamibi is the radio-pharmacological agent of choice, with a sensitivity reported to be between 72%-100% [2]. A recent study has shown that sestamibi combined with ultrasound increases the accuracy of detection for parathyroid adenomas [3].
A number of studies have confirmed that there is both an increased risk of fracture in patients with primary hyperparathyroidism and a reduced risk of fractures in patients who undergo parathyroidectomy [4]. Intraoperative monitoring of parathyroid hormone levels during parathyroid surgery is very helpuful due to the short half-life of parathyroid hormone in the blood stream, it is possible to assess operative success with serum PTH levels intraoperatively. It is also possible to perform recurrent laryngeal monitoring intraoperatively although this is still controversial and neither technique has become standard practice.
- VanderWalde, L.H., Liu, I.L. and Haigh, P.I. (2009) Effect of bone mineral density and parathyroidectomy on fracture risk in primary hyperparathyroidism. World Journal of Surgery, 33, 406-411.
- Shen, W., Sabanci, U., Morita, E.T., Siperstein, A.E., Duh, Q.Y. and Clark, O.H. (1997) Sestamibi scanning is inadequate for directing unilateral neck exploration for first-time parathyroidectomy. Archives of Surgery, 132, 969-976.Â
- Patel, C.N., Salahudeen, H.M., Lansdown, M. and Scarsbrook, A.F. (2010) Clinical utility of ultrasound and 99 mTc sestamibi SPECT/CT for preoperative localization of parathyroid adenoma in patients with primary hyperparathyroidism. Clinical Radiology, 65, 278-287.
- Lang, B. (2009) Minimally invasive thyroid and parathyroid surgery.