
Expert Corner
The sinus tarsi approach in displaced intra-articular calcaneal fracture
 Tim Schepers Tim Schepers Amsterdam, Netherlands |
Since the early nineties the Extended Lateral Approach (ELA) has been the workhorse in the treatment of displaced intra-articular calcaneal fractures. This approach is however hampered by a high percentage of (costly) wound complications [1-4]. There is some evidence suggesting that infectious complications lower overall outcome following the surgical treatment of calcaneal fractures [5]. It is therefore of paramount importance to lower the risks of wound complications.
By combining a less invasive open approach at the level of the talocalcaneal joint with percutaneous reduction of the tuber excellent reduction of the posterior facet and good restoration of overall anatomy (height/width/axis) can be obtained.
The Sinus Tarsi Approach (STA) has regained interest after the article by Ebraheim et al [6]. Since that time several case series and a handful of prospective (randomised) trials have been published on this topic [7-11]. Common findings are a strong reduction in the number of wound complications, similar reduction in anatomy and joint congruity, and at least a similar outcome [12,13]. The wound complications are usually minor and easily treated with conservative measures. Only in a few cases re-operation with wound debridement was needed. No need for (free) flap coverage has been reported as the wound is always closable by primary or secondary intension.
The rate of secondary arthrodesis is similar as in the series treated through the ELA. An additional benefit is that the incision for a secondary subtalar arthrodesis is the same (sinus tarsi) incision as for the initial fracture management.
Starting from 2013 we introduced the STA in our hospital, which rapidly became our primary technique with almost 150 cases in the last three years. Below I will describe our preferred technique in the treatment of displaced intra-articular calcaneal fractures via the sinus tarsi approach in a step-by-step manner. Additional key-images are provided (selected images from different patients).
Surgical technique:
Following general anaesthesia, the patient is lying on a bean-bag on the contra-lateral side. The affected leg is in flexion and elevated using the bean-bag (Figure 1).

Figure 1 - Perioperative view of positioning, the sinus tarsi approach and post-operative coverage
The C-arm approaches from the opposite side.
An ankle-block is given using 20cc (Levo-)Bupivacaine at all five nerves approximately 5cm above the ankle joint. In most patients this ensures enough pain relief immediately post-surgery, at which time they start oral analgesics.
Depending on the surgeon's preference a tourniquet is placed on the lower limb a hand-width below the knee-joint. Depending on the systolic blood pressure it will be inflated between 200 and 250 mmHg during the reduction of the joint (approximately 30 to 45 minutes).
An incision (sinus tarsi approach; STA) is made from the tip of the distal fibula towards the base of the fourth metatarsal. It is usually between 3 to 4 cm.
The peroneal tendons are protected and held plantar-wards. The sural nerve is not explored, but if encountered it is freed up and protected.
The canalis tarsi is debrided by removing Hoke’s fat and ligaments between talus and calcaneus.
With a broad periosteal elevator the brittle lateral wall and soft tissues are separated.
A small distractor with 2.5/3.0 half-pins is subsequently mounted on the fibula (above the tibio-talar joint line) and on the distal part of the tuberosity of the calcaneus. The pin placement is adjusted for any varus/valgus malalignment.
A 1.6mm K-wire is inserted from plantar through the medial sustentaculum part of the fractured calcaneus and driven into the talus to create a constant/fixed part medially.
By increasing distraction the tuberosity is brought downwards and space is created in the posterior talocalcaneal joint. When the fracture is older than 1-1.5 weeks the primary fracture lines sometimes need to be released with small osteotomes.
Depending on the type of the intra-articular fracture (Joint-depression; JD or Tongue-type; TT) different reduction maneuvers are employed.
In case of a JD fracture with the use of a small bone rasp and a small K-wire introduced through the STA as a joystick, the depressed fragments are lifted against the talus and fixated towards the medial constant fragment. Sometimes additional K-wires from plantar are needed to stabilise these fragments prior to definitive fixation. In case of multiple intra-articular fracture-lines one works from medial towards lateral. Reducing the lateral joint fragment last. This should restore Bӧhlers' angle.
In case of a TT a 2.5-3.0mm half-pin is introduced from posterior to lever the fragment in place. Often aided with a small bone rasp or Howard elevator via the STA. Reduction of the joint can be observed via the STA and using image intensifier.
With the foot in neutral position a lateral view can be obtained, when lifting the forefoot (toes higher than heel) a Brodén view is made. With the patient on the contralateral side, by extending the leg, externally rotating at the hip and lifting the forefoot further an axial view can be obtained by aiming the C-arm at 45 degrees towards the sole of the foot.
Subsequently the anterior process and Gissane’s angle are assessed.
At this stage a decision is made whether joint reconstruction is feasible. If the fracture is likely to require secondary arthrodesis in the future (Böhlers' angle below zero degrees, open fractures, Sanders type 4, locked fracture dislocations) a primary arthrodesis has been discussed with the patient pre-operatively as part of the shared discussion making process.
In case of a primary arthrodesis the cartilage is removed from the subtalar joint and three 7.3 cannulated screws are added to the fixation of the calcaneal fracture (Figure 2).

Figure 2 - Example of a severe displaced intra-articular calcaneal fracture treated with a primary arthrodesis following reduction through a sinus tarsi approach
Following anatomical reduction of the joint and temporary K-wire fixation of the calcaneus the lateral wall is reduced.
Now either screw fixation can be performed or a small plate is introduced via the STA. Both methods are combined with longitudinal percutaneous screws from posterior (Figure 3).
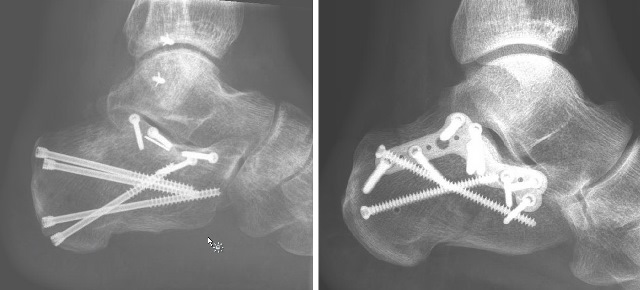
Figure 3 - Two examples of different fixation methods following reduction
Rarely a bone filler is used to fill the cavity of the neutral triangle.
After rinsing the wound, it is closed in layers, with the skin closed with either Donati sutures or a running locked skin closure. Either a pressure bandage for 3 days or a negative pressure wound dressing is applied for 1 week (only in high risk wounds). After this period people are allowed to change the dressings themselves on a daily basis.
No plaster is used, patients are allowed to exercise the ankle joint as soon as possible. Most patients (without additional injuries) are released from hospital the next day.
Patients stay non-weight bearing for 8 weeks, after which new radiographs (lateral, axial, Brodén views) are obtained. In case of sufficient fracture healing patients are allowed to gradually increase weight bearing.
Patients are well informed about the total recovery time of a displaced intra-articular calcaneal fracture, which may take up to 1-1.5 years.
- Agren PH, Wretenberg P, Sayed-Noor AS. Operative versus nonoperative treatment of displaced intra-articular calcaneal fractures: a prospective, randomized, controlled multicenter trial. J Bone Joint Surg Am. 2013;95(15):1351-7.
- Backes M, Schepers T, Beerekamp MS, Luitse JS, Goslings JC, Schep NW. Wound infections following open reduction and internal fixation of calcaneal fractures with an extended lateral approach. Int Orthop. 2014;38(4):767-73.
- Buckley R, Leighton R, Sanders D, Poon J, Coles CP, Stephen D, et al. Open reduction and internal fixation compared with ORIF and primary subtalar arthrodesis for treatment of Sanders type IV calcaneal fractures: a randomized multicenter trial. J Orthop Trauma. 2014;28(10):577-83.
- Griffin D, Parsons N, Shaw E, Kulikov Y, Hutchinson C, Thorogood M, et al. Operative versus non-operative treatment for closed, displaced, intra-articular fractures of the calcaneus: randomised controlled trial. BMJ. 2014;349:g4483.
- Backes M, Schep NW, Luitse JS, Goslings JC, Schepers T. The effect of postoperative wound infections on functional outcome following intra-articular calcaneal fractures. Arch Orthop Trauma Surg. 2015;135(8):1045-52.
- Ebraheim NA, Elgafy H, Sabry FF, Freih M, Abou-Chakra IS. Sinus tarsi approach with trans-articular fixation for displaced intra-articular fractures of the calcaneus. Foot Ankle Int. 2000;21(2):105-13.
- Basile A, Albo F, Via AG. Comparison Between Sinus Tarsi Approach and Extensile Lateral Approach for Treatment of Closed Displaced Intra-Articular Calcaneal Fractures: A Multicenter Prospective Study. J Foot Ankle Surg. 2016;55(3):513-21.
- Kline AJ, Anderson RB, Davis WH, Jones CP, Cohen BE. Minimally invasive technique versus an extensile lateral approach for intra-articular calcaneal fractures. Foot Ankle Int. 2013;34(6):773-80.
- Xia S, Lu Y, Wang H, Wu Z, Wang Z. Open reduction and internal fixation with conventional plate via L-shaped lateral approach versus internal fixation with percutaneous plate via a sinus tarsi approach for calcaneal fractures - a randomized controlled trial. Int J Surg. 2014;12(5):475-80.
- Yeo JH, Cho HJ, Lee KB. Comparison of two surgical approaches for displaced intra-articular calcaneal fractures: sinus tarsi versus extensile lateral approach. BMC Musculoskelet Disord. 2015;16:63.
- Abdelazeem A, Khedr A, Abousayed M, Seifeldin A, Khaled S. Management of displaced intra-articular calcaneal fractures using the limited open sinus tarsi approach and fixation by screws only technique. Int Orthop. 2014;38(3):601-6.
- Schepers T. The sinus tarsi approach in displaced intra-articular calcaneal fractures: a systematic review. Int Orthop. 2011;35(5):697-703.
- Schepers T. Towards uniformity in communication and a tailor-made treatment for displaced intra-articular calcaneal fractures. Int Orthop. 2014;38(3):663-5.









